For many of us, remnants of the pandemic feel like a distant memory. We are back to “normal” – enjoying family gatherings, restaurants and shopping. Even in New York, one of the last COVID-era mandates has come to an end, with masks and face coverings in healthcare facilities no longer required. However, the healthcare system is still dealing with the aftermath, including the impact on physicians.
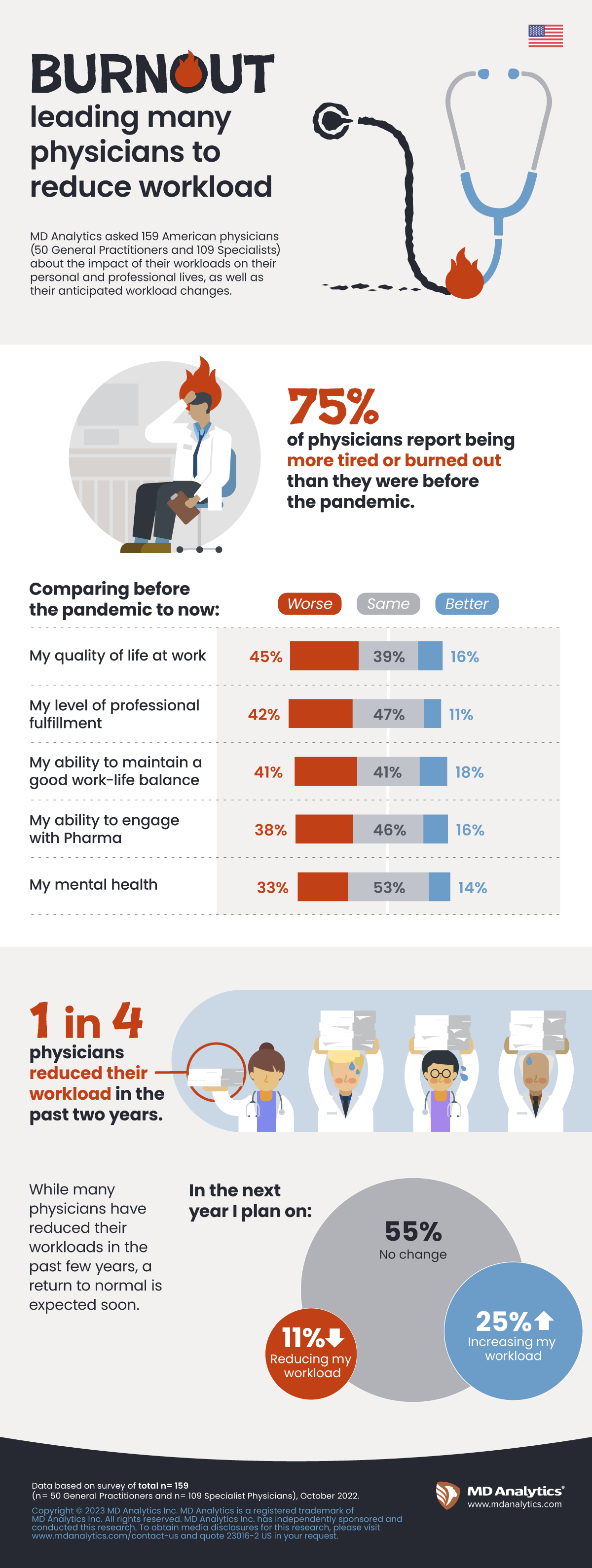
MD Analytics surveyed 50 primary care physicians and 109 specialists about the effect of the COVID crisis on their personal and professional lives. As compared to pre-pandemic, several aspects have gotten worse among physicians:
· Three-fourths say they feel more tired and burnt out.
· One-third say their mental health and level of professional fulfillment has declined.
· Almost one-half say their quality of life at work is worse now.
Read More
Overall, findings are slightly worse for PCPs than specialists. On top of this, one-quarter of both primary care physicians and specialists say they reduced their workload in the past two years – mostly because of burnout, a need for more self-care or staff shortage issues. Some of the main challenges we are hearing anecdotally from hospitals and health systems are staff shortages and physician recruitment and reatinment.
Although one-quarter of physicians say they plan on increasing their workload in the next year, challenges remain. Because of the difficulties in continuing to practice and well-being issues, physicians are either cutting back their hours or leaving the profession altogether.
There is currently a shortage of physicians according to data from the U.S. Health Resources and Services Administration (HRSA). HRSA data shows significant shortages in primary care and psychiatry today, as well as a shortage of general surgeons in rural communities. Furthermore, the U.S. faces a projected shortage of between 37,800 and 124,000 physicians within 12 years according to a recent report a report released by the Association of American Medical Colleges (AAMC).
When it comes to engaging with pharma, a key information source for learning about conditions and treatments, two-fifths of physicians find it more challenging now than pre-pandemic. We can envision how these worsening changes in physicians’ personal and professional lives cascade down to those who are feeling the brunt of it all – patients. We will continue to monitor the environment over the upcoming year to see how the U.S. healthcare system responds.
Key takeaways
- What impact has the COVID crisis had on physicians 3 years later?
- What is the current professional and mental state of our HCPs?