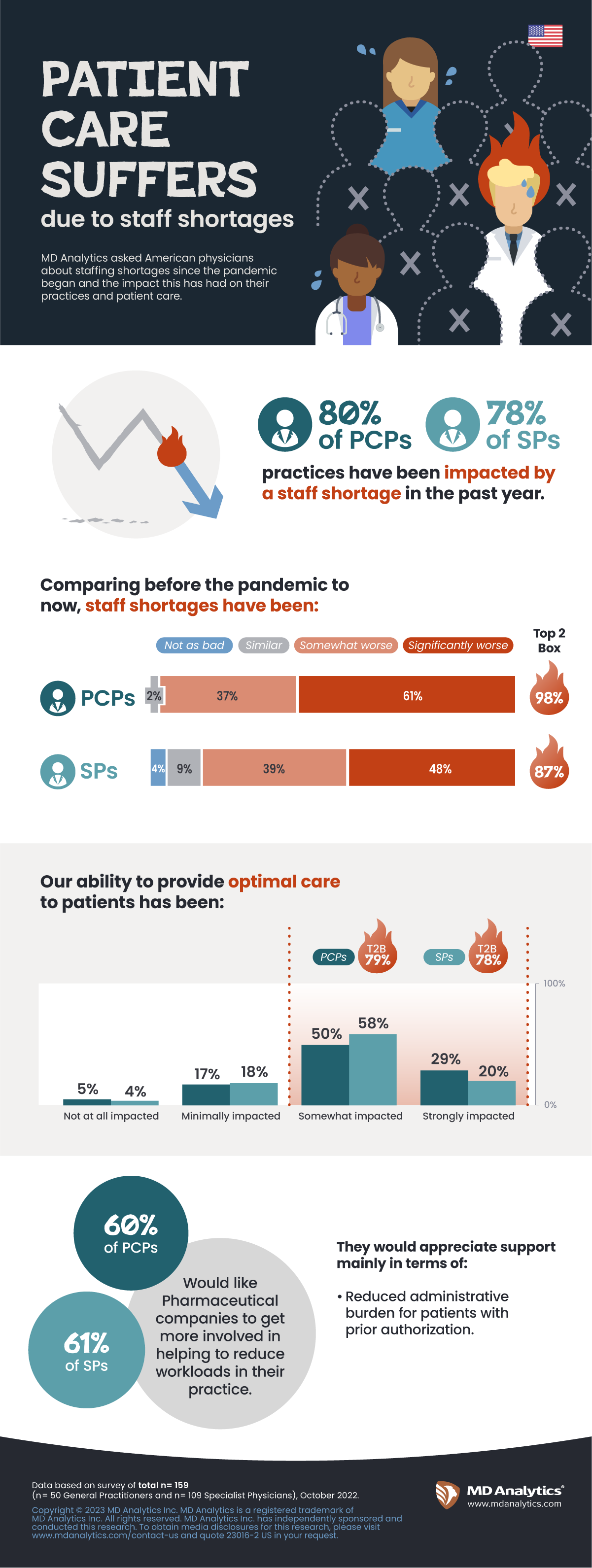
The World Health Organization (WHO) declared the novel coronavirus (COVID-19) outbreak a global pandemic on March 11, 2020. Now at the three-year mark, the US healthcare workforce is still trying to recover and labor shortages are stressing clinicians and hospitals. MD Analytics surveyed 50 primary care physicians and 109 specialists about the effect of the COVID crisis on staff shortages, as well as their attitudes about support from pharmaceutical companies.
In the past year alone, four-fifths of physicians (80% PCPs and 78% Specialists) say they have been impacted by staff shortages, and almost all (98% of PCPs and 87% of Specialists) find the situation worse compared to pre-pandemic. Hospitals (both Teaching and Non-Teaching) are hit the hardest compared to other settings, as well as those in the South relative to other regions.
Read More
Large majorities (79% of PCPs and 78% of Specialists) agree that these staff shortages impact their ability to provide optimal care for patients. Psychiatrists feel most strongly about this, coupling the staff shortages with the increased demand for mental health services stemming from the pandemic. Regardless of specialty, staff shortages continue to be a barrier to patient visits for new diagnoses, treatments, testing and follow-up.
Staffing shortages are expected to continue this year, especially among nurses. Many organizations are still using high-priced contract labor to fill the gaps even as severe COVID-19 hospitalization rates have declined. For example, in December 2022, the national average weekly pay rate for travel nurses was $3,173, according to data from nurse staffing platform Vivian Health. That’s up from $1,894 in January 2020.
In addition, according to Healthcaredive.com, healthcare workers across the country have waged strikes to gain higher pay and optimal staffing conditions in employment contracts, and even resident physicians are increasingly involved in labor organizing. These labor trends will continue to pose challenges to health systems this year as facilities work to get back to pre-pandemic operations and stem labor costs.
How can Pharma help?
Around half (41% PCPs and 55% Specialists) find pharmaceutical companies have been supportive to help alleviate their workloads. Oncologists feel the most supported, Psychiatrists the least. But even more (60% PCPs and 61% Specialists) would like pharmaceutical companies to get more involved to help reduce workloads in their practice.
- The biggest need mentioned across the board: reduced administrative burden for patients with prior authorization.
- Other top needs for Specialists are samples and patient education, whereas PCPs would like more interaction with pharmaceutical representatives.
During the pandemic, many pharma companies launched portals to provide information to physicians and interact with them more directly. While about half of physicians claim to have heard of these, only 1 in 5 have used them thus far. Encouragingly, physicians can see themselves using them in the future:
- Two-fifths (41% PCPs and 37% Specialists) are likely to use company-developed portal/application to support the management of patients.
- Similar proportions (45% PCPs and 37% Specialists) are likely to use of company-developed portal/application to interact with reps/MSLs.
Key takeaways
- Extent to which physicians experienced staff shortages in the last year and how this compares to pre-pandemic conditions
- Assess the role pharmaceutical companies can play in helping alleviate HCP workloads